Inverted papilloma is a benign, epithelial neoplasm originating from the Schneiderian membrane of the nose
and paranasal sinuses. It usually arises from the lateral nasal wall, in the middle meatus, often extending to the ethmoid and maxillary sinuses. In advanced cases, extension into all of the ipsilateral paranasal sinuses may occur, whereas intracranial growth and Dura penetration are rare.
Their characteristic inverted mucosal surface extending into the stroma of the papilloma leads to the term inverted for these lesions. They occur more frequently in men (3:1) and have an incidence of approximately 1 per 100,000 population.
Although benign, they behave in a locally aggressive manner, requiring wide local excision if recurrence is to be prevented. Malignant transformation can occur in up to 10 per cent of lesions but is typically reported as occurring in approximately 2 per cent. The etiology remains unclear, and the reasons for malignant transformation similarly are unknown.
Clinical presentation is typically with unilateral nasal symptoms, especially blockage, rhinorrhoea and epistaxis. Endoscopic examination typically reveals an irregular fleshy lesion arising from the nasal mucosa. The most common site is the lateral nasal wall around the middle turbinate. Bilateral lesions are rare.
Preoperative investigations include CT scanning, which may be complemented by MRI for more detailed soft tissue definition. The extent of the disease will determine the extent of surgery
Staging for IP was proposed by Krouse in 2001:
Stage 1. IPs confined to the nasal cavity
Stage 2. IPs involving the ethmoid sinuses, medial and superior region of maxillary sinus
Stage 3. IPs involving all paranasal sinuses, but confined to the nose and paranasal sinuses
Stage 4. IPs not confined to the nose and paranasal sinuses (i.e. orbital or intracranial extension) or with evidence of malignancy
Histo-Pathology
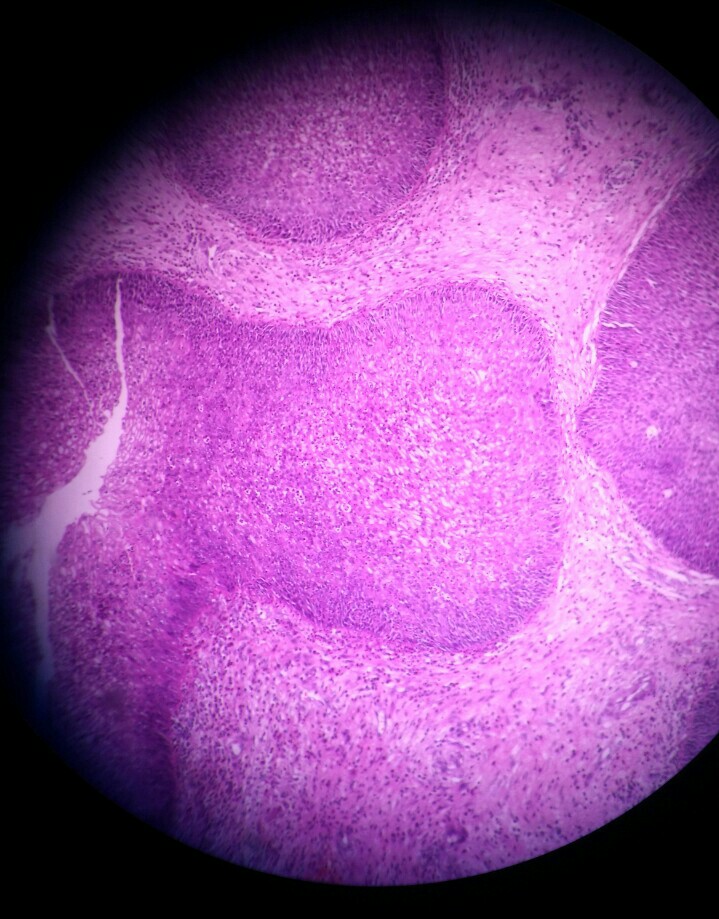 Inverted papillomas are composed of invaginating crypts, cords and nests covered by non-keratinising squamous epithelium, which alternates with columnar ciliated respiratory epithelium and with intermediate or transitional epithelium . This newly formed duct system is similar to the embryonic development of the nasal mucosa. The multilayered epithelium typically contains mucous cells and mucin-filled microcysts. The invagination of the mucosa may result in the presence of apparently discontinuous cell masses lying deep to the epithelial surface, but the basement membrane is intact and may be shown in continuity with that of the surface epithelium. An inverted growth is the hallmark of inverted papilloma, but varying degrees of papillary growth may be seen at the surface. The surface is characteristically lined by a respiratory type of epithelium; nevertheless, foci of surface keratinisation are occasionally present. A few regular mitoses may be found in the basal and parabasal layers. Although the nuclei may show mild nuclear irregularities and hyperchromatism, no disturbances of the cellular polarity are found. An abundant and oedematous connective tissue stroma is a common feature of inverted papillomas. It usually contains macrophages and neutrophils, but eosinophils may also be present. This inflammatory infiltrate may also be present between the epithelial cells, within the dilated lumens of invaginated crypts, and within the numerous microcysts that usually occur in the respiratory epithelium. Seromucinous glands are absent, but branching gland ducts are often present. The tumour grows by extension to involve the contiguous sinonasal epithelium.
Inverted papillomas are composed of invaginating crypts, cords and nests covered by non-keratinising squamous epithelium, which alternates with columnar ciliated respiratory epithelium and with intermediate or transitional epithelium . This newly formed duct system is similar to the embryonic development of the nasal mucosa. The multilayered epithelium typically contains mucous cells and mucin-filled microcysts. The invagination of the mucosa may result in the presence of apparently discontinuous cell masses lying deep to the epithelial surface, but the basement membrane is intact and may be shown in continuity with that of the surface epithelium. An inverted growth is the hallmark of inverted papilloma, but varying degrees of papillary growth may be seen at the surface. The surface is characteristically lined by a respiratory type of epithelium; nevertheless, foci of surface keratinisation are occasionally present. A few regular mitoses may be found in the basal and parabasal layers. Although the nuclei may show mild nuclear irregularities and hyperchromatism, no disturbances of the cellular polarity are found. An abundant and oedematous connective tissue stroma is a common feature of inverted papillomas. It usually contains macrophages and neutrophils, but eosinophils may also be present. This inflammatory infiltrate may also be present between the epithelial cells, within the dilated lumens of invaginated crypts, and within the numerous microcysts that usually occur in the respiratory epithelium. Seromucinous glands are absent, but branching gland ducts are often present. The tumour grows by extension to involve the contiguous sinonasal epithelium.
Specific surgical indication and technique
Inverted papilloma has been associated with a high rate of recurrence between 0 and 78 percent, malignant transformation, residual disease and a tendency towards multicentricity.
‘Recurrence’ actually represents residual disease in most cases, so the basic problem facing the clinician is to determine adequate treatment. Besides the more extended approaches of midfacial degloving, the subcranial approach and more rarely, lateral rhinotomy, the endonasal operation using both microscope and endoscope have grown in importance since the early 1990s. In the case of frontal sinus involvement, the endonasal route is appropriate as long as there are no signs of major bone destruction caused by the tumour and as long there is no significant extension of the neoplasm lateral to a sagittal, vertical plane through the lamina papyracea
It is mandatory to resect not only the tumour, but also to remove the mucoperiosteum in areas from which the tumour originates using the drill. Intraoperative histologic control by frozen section is strongly recommended. Because of the small but definite association with carcinoma (o2 percent), one should separate the specimens according to their different sites of origin to obtain the most detailed mapping of the tumour. It depends on the pneumatization which type of frontal sinus drainage is recommended. In well pneumatized cases a type II drainage is recommended, while in minor pneumatized patients type III drainage provides a sufficient connection between the frontal sinus and the nasal and ethmoidal cavity, which is important to avoid subsequent mucocoele formation.
Statistics and results
There is no statistical evaluation of results after surgery of inverted papillomas of the nasal cavity and paranasal
sinuses with regard to frontal sinus involvement. Early diagnosis and precise identification of lesions by modern imaging techniques has led to an increasing tendency for using the more functional and minimally invasive endonasal approach with both microscope and endoscope.
Waitz and Wigand reported one of the largest and earliest series on 35 patients, who underwent surgery by an intranasal endoscopic approach, with a 17 percent recurrence rate at nearly two years follow up. Comparatively, extranasal approaches in 16 patients resulted in a relapse rate of 19 percent. Endoscopic surgery seems to be successful even in the treatment of large lesions affecting the posterior ethmoidal cells, the nasofrontal recess or the sphenoid sinus. Plinkert et al. recommend that the endonasal approach is reliable for processes restricted to the middle nasal meatus and the anterior ethmoidal cells.
In more recent studies, Stankiewicz and Girgis, McCary et al., Peter and Grossenbacher, \ Tsue et al., Homer et al. and Cooter et al. have documented similar success using the same technique. Brors et al. reported a large series of 37 patients, of whom 33 received endonasal treatment. The follow-up period ranged from 12 months to 10 years, with a mean of 3.4 years. The overall recurrence rate was 16.2 percent (six of 37) and revision surgery was necessary in six cases between one and three years after the first operation. Malignant changes were histologically diagnosed in three cases.
Between January 1992 and September 2000, Tomenzoli et al. collected a series of 47 patients with inverted
papillomas undergoing endoscopic resection. Massive skull base erosion, intradural and intraorbital extension, extensive involvement of the frontal sinus, abundant scar tissue due to previous surgery and concomitant presence of squamous cell carcinoma were considered absolute contraindications for a purely endoscopic approach. Up to September 2000, no recurrences were observed with a mean follow up of 39 months (range, 24–130 months).
Clinical Series
Case 1
A patient named Srinivasulu presented to the Department of ENT, Kurnool Govt general Hospital




















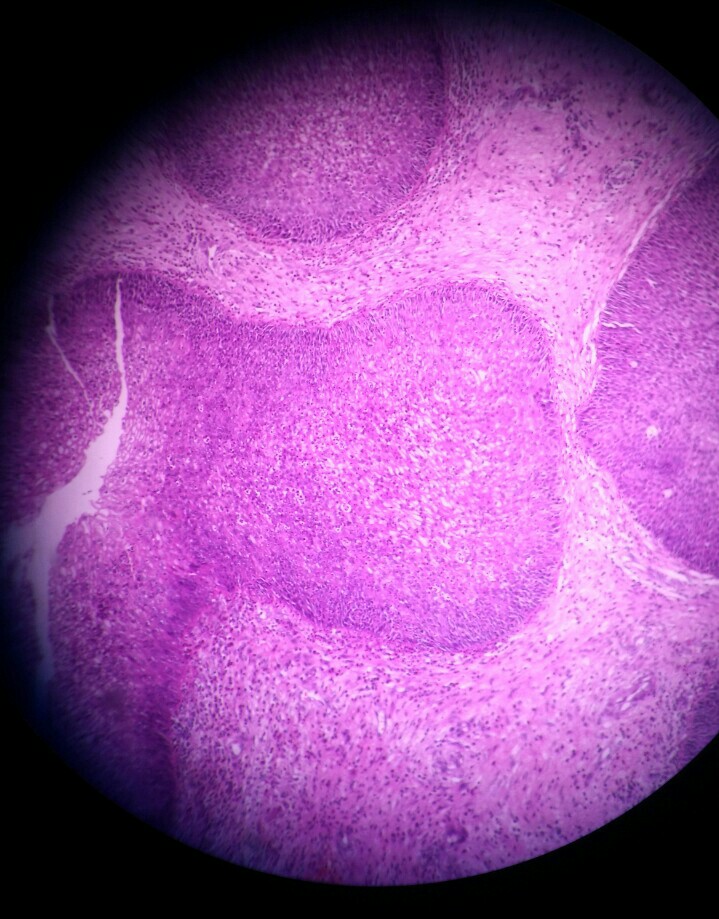 Inverted papillomas are composed of invaginating crypts, cords and nests covered by non-keratinising squamous epithelium, which alternates with columnar ciliated respiratory epithelium and with intermediate or transitional epithelium . This newly formed duct system is similar to the embryonic development of the nasal mucosa. The multilayered epithelium typically contains mucous cells and mucin-filled microcysts. The invagination of the mucosa may result in the presence of apparently discontinuous cell masses lying deep to the epithelial surface, but the basement membrane is intact and may be shown in continuity with that of the surface epithelium. An inverted growth is the hallmark of inverted papilloma, but varying degrees of papillary growth may be seen at the surface. The surface is characteristically lined by a respiratory type of epithelium; nevertheless, foci of surface keratinisation are occasionally present. A few regular mitoses may be found in the basal and parabasal layers. Although the nuclei may show mild nuclear irregularities and hyperchromatism, no disturbances of the cellular polarity are found. An abundant and oedematous connective tissue stroma is a common feature of inverted papillomas. It usually contains macrophages and neutrophils, but eosinophils may also be present. This inflammatory infiltrate may also be present between the epithelial cells, within the dilated lumens of invaginated crypts, and within the numerous microcysts that usually occur in the respiratory epithelium. Seromucinous glands are absent, but branching gland ducts are often present. The tumour grows by extension to involve the contiguous sinonasal epithelium.
Inverted papillomas are composed of invaginating crypts, cords and nests covered by non-keratinising squamous epithelium, which alternates with columnar ciliated respiratory epithelium and with intermediate or transitional epithelium . This newly formed duct system is similar to the embryonic development of the nasal mucosa. The multilayered epithelium typically contains mucous cells and mucin-filled microcysts. The invagination of the mucosa may result in the presence of apparently discontinuous cell masses lying deep to the epithelial surface, but the basement membrane is intact and may be shown in continuity with that of the surface epithelium. An inverted growth is the hallmark of inverted papilloma, but varying degrees of papillary growth may be seen at the surface. The surface is characteristically lined by a respiratory type of epithelium; nevertheless, foci of surface keratinisation are occasionally present. A few regular mitoses may be found in the basal and parabasal layers. Although the nuclei may show mild nuclear irregularities and hyperchromatism, no disturbances of the cellular polarity are found. An abundant and oedematous connective tissue stroma is a common feature of inverted papillomas. It usually contains macrophages and neutrophils, but eosinophils may also be present. This inflammatory infiltrate may also be present between the epithelial cells, within the dilated lumens of invaginated crypts, and within the numerous microcysts that usually occur in the respiratory epithelium. Seromucinous glands are absent, but branching gland ducts are often present. The tumour grows by extension to involve the contiguous sinonasal epithelium.